Chapter 17
Physiology of the Kidneys
Chapter Scope
Imagine yourself at home attaching a plastic tube that protrudes from an opening in the skin over your abdomen to a similar connector tube of a portable machine. Then you turn on the machine that begins pumping several liters of sterile salt solution into your abdominal cavity between the abdominal membranes and the internal organs. As time passes, the thin membrane (peritoneum) that covers these organs filters your blood wastes. As they diffuse from the capillaries into your fluid-filled abdominal cavity, theses waste molecules are then drained with the salt solution out through the plastic tubes and discarded. This ordeal describes home peritoneal dialysis for people whose kidneys do not function properly. Repeated several times each day, this procedure consumes many hours and is very expensive.
Filtration of the blood is only part of the work normally done by healthy kidneys. Much of the work of the kidneys is spent in the return of filtered substance to the blood — a process called reabsorption. Requiring an enormous amount of energy, reabsorption rescues many filtered, but important solutes such as sodium ion (Na+), potassium ion (K+), bicarbonate ion (HCO3-), glucose, amino acids; and gas such as carbon dioxide (CO2); and, of course, the solvent, water. Meanwhile, those substances that are filtered but not reabsorbed remain in the nephron tubules to join additional substances that have been added to the nephron by way of the third major function of the kidney, secretion. Secretion provides the kidney with an alternate mechanism for ridding the body of specific molecules (in addition to filtration), by moving substances that were not filtered out of the blood and into the nephron tubules at a site downstream from the glomerulus. Together, with a minimum amount of obligatory water, these wastes are excreted as urine. Through these three functions — filtration, reabsorption, and secretion — the kidneys are able to eliminate potentially toxic atoms of nitrogen (as urea) from the metabolism of proteins (chapters 2, 5). The kidneys also retrieve small electrolytes like Na+, K+, and H+ which have slipped through the glomerular filter, regulate the overall body pH, and adjust the circulating water volume in the body. Be sure to notice the important role of the kidneys in the manipulation of hydrogen ions (H+) and bicarbonate ions (HCO3-) as they maintain the body’s acid-base balance (see chapter 16 for discussion of the equally important respiratory influence on acid-base balance).
The kidneys are involved in regulating the total volume of water in the body. During conditions of dehydration when the total water volume is too low, osmoreceptors located in the hypothalamus are activated and antidiuretic hormone (ADH) is secreted from storage vesicles in the posterior pituitary. Through its action on the walls of the nephron tubules, ADH promotes the reabsorption of water from the nephron tubules to restore the body fluid levels. By contrast, when body water is too high such as in hypertension or in patients with excess water in the tissues (edema), different types of diuretic drugs may be prescribed that act on specific regions of the nephron tubule to inhibit water reabsorption. Such diuretics promote the loss of extra water in the urine. Other hormones that act on the kidney include aldosterone that is secreted by the adrenal cortex primarily to reabsorb sodium and atrial natriuretic peptide (ANP) that opposes aldosterone by promoting the excretion of sodium in the urine.
I. Structure and Function of the Kidneys
Each kidney contains many tiny tubules that empty into a cavity drained by the ureter. Each of the tubules receives a blood filtrate from a capillary bed called the glomerulus. The filtrate is similar to tissue fluid, but it is modified as it passes through different regions of the tubule and is thereby changed into urine. The tubules and associated blood vessels thus form the functioning units of the kidneys, known as nephrons.
A. Multiple Choice
- Which of the following activities is not regulated by the kidneys?
- a. the volume of blood plasma, and thus, blood pressure
- b. waste product concentrations in the blood
- c. certain electrolyte concentrations in the blood
- d. the acid-base balance (pH) of the blood plasma
- e. All of these activities are regulated by the kidneys.
- The structure of the kidney reveals that the
- a. medulla is in contact with the outer capsule
- b. medulla is divided into eight to fifteen conical renal pyramids
- c. cortex drains into the minor calyces
- d. urethra transports urine to the urinary bladder
- e. female urethra is longer than the male urethra
- Which statement about the micturition process is false?
- a. It is controlled by a reflex center located in the sacral levels of the spinal cord.
- b. Stretch receptors in the bladder initiate this reflex when the bladder volume of urine reaches a critical minimum.
- c. Firing of the reflex centers results in simultaneous contraction of the detrusor muscle and relaxation of the internal urethral sphincter, pressuring urine into the urethra.
- d. The urge to urinate, reflexly stimulates the autonomic nerves to contract the external sphincter so that urine is not accidentally released.
- e. All of these statements regarding micturition are true.
- The vessel delivering blood directly to the glomerulus is the
- a. renal artery
- b. interlobar artery
- c. arcuate artery
- d. interlobular artery
- e. afferent arteriole
- Which statement about the kidney vasculature is false?
- a. The kidney has two capillary beds that arranged such that the glomerular capillary bed is drained by an arteriole rather than a venule.
- b. All blood entering the kidney is completely filtered in the glomerulus and forms filtrate that is later returned to the veins by reabsorption.
- c. Peritubular capillaries are the kidney’s “real” capillaries since they function in the exchange of gases and nutrients for wastes.
- d. The efferent arteriole contains blood that has been filtered and is leaving the glomerulus.
- e. All of these statements regarding kidney vasculature are true.
- The section of the nephron consisting of a single layer of cuboidal cells with microvilli to increase the surface area for reabsorption, is known as the
- a. glomerular capsule
- b. proximal tubule
- c. loop of Henle
- d. distal tubule
- e. collecting duct
B. True or False/Edit
- The primary function of the kidney is the regulation of the intracellular fluid environment in the body.
- The internal urethral sphincter (the upper sphincter) is composed of smooth muscle, whereas the external urethral sphincter (the lower sphincter) is composed of skeletal muscle and thus its voluntary control is learned early in life.
- The functional unit of the kidney that is responsible for the formation of urine is called the renal pyramid.
- The glomerulus is the structure that is thought of as the “filter” of the kidney since it forms a unique fluid called filtrate from blood.
- The glomerulus, the glomerular capsule, and the proximal convoluted tubule are all located within the medulla region of the kidney.
- There are two types of nephrons, which are classified according to their position and the lengths of their loops of Henle.
- The kidney filtrate becomes urine only when is passes through the distal tubules and enters the collecting ducts.
II. Glomerular Filtration
- The glomerular capillaries have large pores in their walls, and the layer of Bowman’s capsule in contact with the glomerulus has filtration slits. Water, together with dissolved solutes (but not proteins) can thus pass from the blood plasma to the inside of the capsule and the nephron tubules. The volume of this filtrate produced by both kidneys per minute is called the glomerular filtration rate (GFR).
A. Multiple Choice
- Which substance is filtered by the glomerulus and thus is found in the nephron ultrafiltrate?
- a. red blood cells
- b. platelets
- c. proteins
- d. white blood cells
- e. electrolytes
- The net filtration pressure at the glomerulus that results in the formation of ultrafiltrate is
- a. about equal to arterial blood pressure at 100 mmHg
- b. partially due to the very low colloid osmotic pressure of plasma
- c. opposed by the high osmotic pressure of ultrafiltrate
- d. estimated to be approximately 10 mmHg
- Which statement about the glomerular filtration rate (GFR) is false?
- a. GFR averages approximately 180 L (about 45 gallons) per day.
- b. GFR will increase during fight‑or‑flight situations due to the vasodilation of afferent arterioles.
- c. A decrease in GFR results in a decrease in the total urine output.
- d. Renal autoregulation maintains the GFR at a relatively constant rate despite fluctuations in the mean arterial blood pressure.
B. True or False/Edit
- Proteins can pass through the glomerular capillary pores yet do not appear in the filtrate mainly because they are too large to pass through the basement membrane outside the capillary wall and are repelled by membrane’s negative charges.
- Our total urine production each day is greater than our daily glomerular filtration rate (GFR).
- A fall in systemic arterial blood pressure toward 70 mmHg releases locally produced chemicals that dilate the afferent arterioles, thus keeping the GFR relatively constant (renal autoregulation).
- When blood pressure falls, sympathetic (fight-or-flight) nerve activity vasoconstricts afferent arterioles while renal autoregulation (local) vasodilates afferent arterioles.
- The tubuloglomerular feedback process describes how specialized cells of the macula densa portion of nephron tubule sense any increased flow of filtrate and signal the incoming afferent arteriole to constrict; thus lowering the GFR and reducing the flow of filtrate (a form of negative feedback)
III. Reabsorption of Salt and Water
- Most of the salt and water filtered from the blood is returned to the blood through reabsorption through the wall of the proximal tubule. The reabsorption of water occurs by osmosis, in which water follows the transport of NaCl from the tubule into the surrounding capillaries. Most of the water remaining in the filtrate is reabsorbed across the wall of the collecting duct in the renal medulla. This occurs as a result of the high osmotic pressure of the surrounding tissue fluid, which is produced by transport processes in the loop of Henle.
A. Multiple Choice
- The return of filtered molecules from the tubules to the blood is called
- a. filtration
- b. reabsorption
- c. secretion
- d. excretion
- e. None of these terms is correct.
- Which event does not occur in the proximal tubule section of the kidney nephron?
- a. Na+ is actively pumped across the basal membranes and out of the epithelial cells.
- b. From a higher concentration in the filtrate, Na+ diffuses passively toward a lower concentration in the epithelial cells.
- c. Cl- follows Na+ passively from the filtrate and into the epithelial cells.
- d. Reabsorption of dissolved solutes leaves the remaining filtrate entering the loop of Henle very hypotonic.
- e. All of these events occur in the proximal tubule.
- Which of these statements about the proximal tubule is false?
- a. Sixty-five percent of the original glomerular ultrafiltrate is reabsorbed here and returned to the blood.
- b. Here, hormones do not regulate reabsorption.
- c. Although ATP is consumed, the overall energy expenditure here is small.
- d. The tubular fluid entering the loop of Henle remains isosmotic with blood at about 300 mOsm.
- Which event does not occur in the ascending portion of the loop of Henle?
- a. Na+, K+, and Cl- are all actively pumped from the filtrate into the ascending limb cells.
- b. Na+ is actively pumped across the basolateral membranes of the epithelial cells to the tissue fluid.
- c. By passive electrical attraction, Cl- follows the Na+.
- d. K+ passively diffuses back into the filtrate or out the basolateral membrane.
- e. Water diffuses passively (osmosis) and is reabsorbed, following the ions across the walls of the ascending limb.
- Which statement regarding the countercurrent multiplier system is false?
- a. The descending limb of the loop of Henle is seemingly permeable to salt and other dissolved solutes, forming a hypertonic filtrate.
- b. Interaction between ascending and descending tubular flow in the loop of Henle is an excellent example of negative feedback.
- c. Salt becomes recirculated and trapped in the medullary interstitial tissue fluid, increasing in “saltiness” as it accumulates toward the lower tip of the pyramids.
- d. Water is removed from the medulla by the higher colloid osmotic pressure of the blood in the vasa recta capillaries.
- e. Urea is recycled by passively diffusing out of the collecting duct specific urea transporters, through the medullary tissue, and into the ascending limb.
- When the concentration of antidiuretic hormone (ADH) rises in the blood
- a. the walls of the collecting ducts become less permeable to dissolved solutes and water
- b. water channels appear along the collecting duct epithelial cells as vesicles containing proteins called aquaporins arise from the Golgi apparatus and fuse to the epithelial cell membranes
- c. the ultrafiltrate flowing through the collecting duct becomes more hypotonic
- d. a greater volume of dilute urine is excreted
- e. None of these statements regarding ADH is correct.
- Antidiuretic hormone (ADH)
- a. is synthesized by neurons of the hypothalamus and released from the posterior pituitary gland
- b. binds to receptors on the collecting ducts cells and activates a cAMP second messenger system
- c. is released during body dehydration conditions to place aquaporin proteins (water channels) along the collecting duct, promoting water retention
- d. is released when osmoreceptors in the hypothalamus sense an increase in the blood osmotic pressure (osmolality)
- e. All of these statements regarding ADH are correct.
B. True or False/Edit
- Only 400 ml of urine per day (known as the obligatory water loss) is required to excrete the metabolic wastes produced by the body.
- Reabsorption is the movement of filtered water and molecules from the nephron tubules, through the tubular epithelial cells and eventually into the blood.
- The osmolality of the filtrate is essentially the same as that of plasma at 300 mOsm/L and is thus isosmotic with the plasma.
- In the proximal tubule, the Na+/K+ pumps are located along both the apical and basal sides of the epithelial cell membranes.
- Nearly two-thirds of salt and water in the original ultrafiltrate is reabsorbed from the proximal tubule and returned to the blood.
- The total metabolic cost for reabsorption in the proximal tubule and the loop of Henle is very high — about 6% of the total calories required by the average adult every day.
- For water reabsorption (osmosis) to occur from the filtrate, the tissue fluid flowing outside the nephron between the interstitial cells of the renal medulla must be hypotonic.
- Tubular fluid leaving the loop of Henle and entering the distal tubule in the kidney cortex is hypotonic (about 100 mOsm/L) whereas the tissue fluid in the medulla is made hypertonic.
- Because proteins (colloids) are present in the blood but not in the medullary fluid, water flows from the medulla into the peritubular (vasa recta) capillaries, thus removing water from the renal medulla.
- Normally, 99.2% of the 180 L of glomerular ultrafiltrate is reabsorbed in the nephrons so that only 1.5 L of urine is excreted per day.
C. Label the Figure ‑‑ Urea and Sodium Flow in the Countercurrent Multiplier System
- Figure 17.18 in the text is a summary of some very complex solute and fluid movements into and out of the loop of Henle and collecting tubule portions of the kidney nephron. Starting with the cortex region in the upper left corner of figure 17.1 below, fill in the proper term(s) or chemical symbol(s) in the blank spaces provided. Think of the properties each portion of the nephron epithelium must possess to cause the net movements you are labeling. This will be a valuable visual aid to help your review of the countercurrent multiplier system when studying for an exam. Check your work against the figure in the text. Good luck!
- Figure 17.18 The role of urea in urine concentration. Urea diffuses out of the inner collecting duct and contributes significantly to the concentration of the interstitial fluid in the renal medulla. The active transport of Na+ out of the thick segments of the ascending limbs also contributes to the hypertonicity of the medulla, so that water is reabsorbed by osmosis from the collecting ducts.
IV. Renal Plasma Clearance
- As blood passes through the kidneys, some of the constituents of the plasma are removed and excreted in the urine. The blood is thus “cleared,” to some extent, of particular solutes in the process of urine formation. These solutes may be removed from the blood by filtration through the glomerular capillaries or by secretion by the tubular cells into the filtrate. At the same time, certain molecules in the tubular fluid can be reabsorbed back into the blood.
A. Multiple Choice
- Which statement about renal clearance is false?
- Renal clearance results only in the removal of urea from the blood.
- Renal clearance removes filtered molecules and ions from the blood.
- Renal clearance is dependent upon filtration at the glomerulus.
- The process of secretion increases the net renal clearance.
- The process of reabsorption reduces the net renal clearance.
- Substances that are secreted by the kidneys
- are moving in the opposite direction of reabsorption.
- move out of the peritubular capillaries and into the interstitial fluid.
- are transported across the basolateral membrane of the tubular epithelial cells
- are transported into the lumen of the nephron tubule for excretion.
- All of these statements describe the secretion of substances by the kidneys.
- Which statement about penicillin is false?
- Penicillin is an antibiotic first used during World War II.
- Penicillin can be administered in low doses because it is actively reabsorbed.
- Penicillin is secreted by the kidney nephron tubules.
- Penicillin effectiveness can be increased by probenecid, an inhibitor of the organic anion transporters located along the proximal tubule.
- Which statement about inulin is false?
- a. Inulin is a polymer of fructose, a simple sugar.
- b. Inulin is easily filtered by the glomerulus of the nephron.
- c. Inulin is not reabsorbed by the walls of the nephron.
- d. Inulin is not secreted by the walls of the nephron.
- e. All of these statements about inulin are true.
- Which plasma molecule is filtered and then completely (100%) reabsorbed by the nephron?
- a. protein
- b. inulin
- c. urea
- d. glucose
- e. creatinine
- Which plasma molecule is both filtered and secreted by the nephron? [hint: used to measure the renal blood flow]
- a. potassium ion (K+)
- b. inulin
- c. urea
- d. glucose
- e. para-aminohippuric acid (PAH)
- Which plasma substance is filtered, reabsorbed, and secreted by the nephron?
- a. potassium ion (K+)
- b. inulin
- c. urea
- d. glucose
- e. para-aminohippuric acid (PAH)
- Which statement about the movements of glucose and amino acids within the kidney nephron is false?
- a. They are easily filtered by the glomeruli into the renal tubules of the nephrons.
- b. They are normally not found in the urine.
- c. They are reabsorbed into the nephron tubule cells by primary rather than secondary active transport.
- d. They are reabsorbed completely until their concentrations exceed their transport maximum (Tm).
- e. They are able to saturate their membrane carriers and appear in the urine if their renal plasma thresholds are exceeded.
B. True or False/Edit
- Renal clearance refers to the ability of the kidneys to remove molecules from the blood plasma by excreting them in the urine.
- Secretion is the movement of plasma solutes in a direction opposite to that of reabsorption.
- Xenobiotics are molecules foreign to the body – such as toxins and drugs –that can be eliminated rapidly from the blood by “polyspecific” organic anion transporters located along the proximal tubule of the kidney nephron.
- The amount of inulin passing into the urine and excreted each minute is exactly equal to the glomerular filtration rate (GFR).
- Renal plasma clearance can be defined as the volume of plasma from which a substance is completely removed or “cleared” in one minute by excretion in the urine.
- If a substance is secreted into the nephron, its plasma clearance rate is less than the glomerular filtration rate (GFR).
- Urea, formed in the liver from amino acids during protein metabolism, is filtered at the glomerulus and is partially reabsorbed along the nephron.
- Blood entering the kidneys through the renal artery will be completely free of all wastes when it exits the kidneys through the renal vein.
- The plasma clearance of para‑aminohippuric acid (PAH) can be used to measure the total renal blood flow in ml per minute.
- Roughly 80% of the total renal plasma flow is filtered at the glomerulus; while the remaining 20% passes on to the efferent arterioles.
- The appearance of glucose in the urine (glycosuria) occurs only when the plasma concentration of glucose is abnormally high (hyperglycemia), exceeding its renal plasma threshold.
- Diabetes mellitus is a disease characterized by the inadequate secretion or action of insulin resulting in hypoglycemia (measured after fasting) and glycosuria.
- Diabetes insipidus and diabetes mellitus are similar diseases, differing only in severity of their symptoms.
V. Renal Control of Electrolyte and Acid-Base Balance
- The kidneys regulate the blood concentration of Na+, K+, HCO3-, and H+. Aldosterone stimulates the reabsorption of Na+ in exchange for K+ in the tubule. Aldosterone thus promotes the renal retention of Na+ and the excretion of K+. Secretion of aldosterone from the adrenal cortex is stimulated directly by a high blood K+ concentration and indirectly by a low Na+ concentration via the renin‑angiotensin system.
A. Multiple Choice
- Which electrolyte is not regulated mainly by the action of the kidneys on the blood?
- a. sodium
- b. potassium
- c. iron
- d. bicarbonate
- e. phosphate
- Which statement about aldosterone is false?
- a. Aldosterone is a major steroid (mineralocorticoid) hormone secreted by the kidney.
- b. Aldosterone promotes the reabsorption of Na+ in the late distal tubule and the cortical region of the collecting duct.
- c. Aldosterone stimulates the secretion of K+ from the peritubular blood into the distal tubule.
- d. Too much aldosterone secretion can result in hypokalemia.
- e. A fall in blood volume can result in the indirect increase in aldosterone secretion.
- Which statement about the juxtaglomerular apparatus (JGA) of the kidney is false?
- a. The JGA is a location in each nephron where the afferent arteriole and the distal convoluted tubule contact each other.
- b. The role of the JGA macula densa region of the distal tubule is to secrete the enzyme renin.
- c. The JGA granular cells within the afferent arteriole are sensitive to renal blood flow (acting as baroreceptors?).
- d. High Na+ concentrations in the filtrate can inhibit the secretion of renin from the JGA.
- e. All of these statements regarding the JGA are true.
- Which homeostatic response to a high blood volume would not likely occur?
- a. a decrease in renin secretion
- b. a decrease in aldosterone secretion
- c. a decrease in atrial natriuretic peptide (ANP) secretion
- d. an increase in Na+ excretion in the urine
- e. an decrease in antidiuretic hormone (ADH) secretion.
- Which statement about the role of the kidneys the regulation of normal blood pH is false?
- a. The kidneys work to excrete bicarbonate ion in the urine and to reabsorb hydrogen ion .
- b. Hydrogen ion (H+) can enter the filtrate in two ways: by filtration through the glomerulus and by tubular secretion.
- c. Most of the hydrogen ion (H+) secretion occurs across the wall of the proximal tubule in exchange for the reabsorption of sodium ion (Na+).
- d. Buffers, like bicarbonate ion, can bind and release free H+ when necessary, thus stabilizing pH.
- e. Normal urine has little bicarbonate and is slightly acidic, with a pH range between 5 and 7.
- Which statement about the reabsorption of bicarbonate in the proximal tubule is false?
- a. The apical membranes of the tubule cells are impermeable (do not allow diffusion) to bicarbonate.
- b. Bicarbonate in the filtrate is converted to carbon dioxide and water by the action of the enzyme, carbonic anhydrase.
- c. The enzyme, carbonic anhydrase, is located both in the apical cell membrane and in the tubule cell cytoplasm.
- d. During alkalosis, less bicarbonate is reabsorbed and more bicarbonate is excreted to help stabilize the pH.
- e. All of these statements regarding bicarbonate reabsorption in the proximal tubule are true.
- The two organs most responsible for acid-base balance are the
- a. heart and kidneys
- b. liver and lungs
- c. kidneys and lungs
- d. lungs and heart
- e. liver and heart
- Which statement about acid-base regulation in the kidneys is false?
- a. The kidneys can filter and secrete H+ into the filtrate.
- b. The kidneys normally reabsorb all bicarbonate ion filtered at the glomerulus.
- c. Normally some H+ is excreted each day in the urine, thus lowering the urine pH value
below 7.
- d. Filtered bicarbonate present in the filtrate is reabsorbed into the blood indirectly as CO2 gas.
- e. All of these statements about acid-base regulation in the kidneys are true.
B. True or False/Edit
- Approximately 90% of the filtered Na+ and K+ is reabsorbed without the influence of hormones in the early part of the nephron, closer to the glomerulus.
- In the absence of aldosterone, an impressive 2% of the filtered Na+ (roughly 30 g) will be excreted with the urine each day.
- Aldosterone works to reabsorb sodium primarily in the proximal convoluted tubule and in the cortical region of the collecting duct.
- The action of aldosterone on the nephron is the only means by which the body can get rid of any excess plasma potassium (K+).
- Cardiac arrhythmias, and even death, can occur when plasma K+ concentrations are either abnormally high or abnormally low.
- A rise in plasma Na+ concentration directly stimulates the secretion of aldosterone from the adrenal cortex.
- Renin and angiotensin converting enzyme (ACE) are the only two enzymes in the renin-angiotensin-aldosterone system.
- The macula densa cells of the juxtaglomerular apparatus (JGA) act to inhibit renin and aldosterone secretion when the blood and filtrate Na+ concentrations are raised.
- During severe acidosis an increase in H+ secretion into the distal tubule will take the place of K+ as Na+ is reabsorbed, leading to a rise in blood K+ levels (hyperkalemia).
- Bicarbonate ion (HCO3-) is a buffer to which free H+ can bind, thus causing the H+ concentration to fall and the pH to rise.
- In the regulation of whole body pH, the lungs are primarily responsible for the control of bicarbonate ions whereas the kidneys are primarily responsible for the control of carbon dioxide levels in the blood.
- Given a normal level of bicarbonate ion in the blood (21-26 mEq/L), a rise in PCO2 levels greater than 45 mmHg results in a respiratory alkalosis.
- A blood pH lower than 7.35 due to high PCO2 is called a respiratory acidosis.
- The enzyme, carbonic anhydrase, is located on the apical membrane and in the cytoplasm of proximal tubule cells.
- In order for bicarbonate ion to be reabsorbed from the filtrate and returned into the blood, it must first combine with carbon dioxide gas.
- Most of the H+ that is excreted in the urine is first combined (and buffered) to either phosphates (HPO4-2) or ammonia (NH3) molecules.
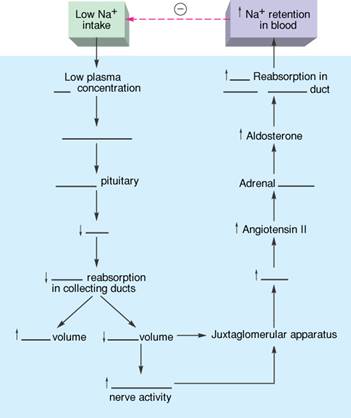
C. Label the Figure – Homeostasis of Plasma Sodium
The maintenance of sodium ion (Na+) levels in the blood plasma is a beautiful example of a functioning negative feedback system (homeostasis). In figure 17.26 in the text, the fall in blood sodium levels due to a low sodium dietary intake is sensed by receptors in the hypothalamus, and specific pathways are activated to restore sodium levels by promoting the reabsorption of Na+ from the kidney filtrate. The last leg of this pathway involves the renin-angiotensin-aldosterone mechanism originating in the nephron of the kidney. Test your understanding of this important series of events by completing the flowchart in figure 17.2 below. Remember, most homeostatic mechanisms in the body can be demonstrated using a similar flowchart format; some simpler and others more complex. Notice that if you start with a high Na+ intake, you can follow the same flowchart; however, the arrows must be reversed along the way. Try it!
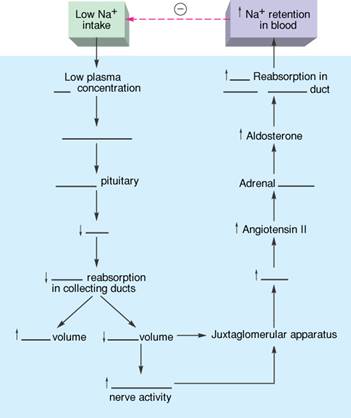
Figure 17.2 This is the sequence of events by which a low sodium (salt) intake leads to increased sodium reabsorption by the kidneys. The dashed arrow and negative sign at the top indicate the completion of the negative feedback loop.
VI. Clinical Applications
Different types of diuretic drugs act on specific segments of the nephron tubule to indirectly inhibit the reabsorption of water and thus promote the lowering of blood volume. A knowledge of how diuretics exert their effects thus enhances understanding of the physiology of the nephron. Clinical analysis of the urine, similarly, is meaningful only when the mechanisms that produce normal urine composition are understood.
A. Multiple Choice
- The purpose for taking diuretic drugs as medication is to
- a. lower blood volume
- b. lower blood pressure
- c. treat congestive heart failure
- d. reduce edema
e. All of these conditions can benefit from diuretic drug medication.
- The most powerful diuretics, inhibiting salt and water reabsorption by as much as 25%, are
- a. carbonic anhydrase inhibitors
- b. loop diuretics
- c. thiazide diuretics
- d. potassium-sparing diuretics
- Diuretics that competitively block the aldosterone-induced stimulation of Na+ reabsorption and K+ secretion in the distal tubule, are the
- a. carbonic anhydrase inhibitors
- b. loop diuretics
- c. thiazide diuretics
- d. potassium-sparing diuretics
- The major kidney function that can not be performed by artificial dialysis membranes is to
- a. separate molecules on the basis of size
- b. prevent the diffusion of plasma proteins
- c. reabsorb Na+, K+, glucose, and other molecules
- d. allow the free movement of water (solvent)
- e. Dialysis membranes perform all of these functions.
B. True or False/Edit
- Clinically, one of the most important kidney functions involves the ability of the kidneys to regulate blood volume in the management of high blood pressure.
- That part of the nephron where most diuretic drugs act to promote water loss is the proximal convoluted tubule.
- The carbonic anhydrase inhibitors like acetazolamide are much more powerful diuretics than the loop diuretics like furosemide (Lasix) and ethacrynic acid.
- Potassium-sparing diuretics may be used in place of other diuretics when there is a risk of excess K+ secretion into the filtrate and its excessive elimination in the urine; resulting in hypokalemia.
- Glomerulonephritis is currently believed to be an autoimmune disease which involves the person’s own antibodies.
- Hemodialysis is a procedure that can be performed by a patient several times a day at home, whereas continuous ambulatory peritoneal dialysis (CAPD) is commonly performed three times a week for several hours each session.
Chapter Review
A. Crossword Puzzle — Physiology of the Kidneys
Across
2. proximal tubule membrane surface with Na+ active transport pumps
4. all nephrons originate here
6. drug used to measure the total renal blood flow
7. approximately 65% of filtrate, salt, and water reabsorbed in this portion of the nephron
9. the “filter” of the kidney nephron
12. reabsorption of water occurs by this process
14. abbreviation of the enzyme that combines carbon dioxide and water; helps acid-base balance
16. abbreviation describing the point at which all reabsorption carrier molecules are saturated
17. hypothalamic hormone responsible for water reabsorption in the collecting duct of the nephron
18. another name for an electrolyte
19. the kidney medulla is divided into wedges known as ________
21. the working functional unit of the kidney is called the ________
22. proximal tubule carriers reabsorb all glucose and ________ acids from the ultrafiltrate
23. ________recta capillaries in the medulla help establish the countercurrent multiplier system
24. adrenal cortex hormone that promotes Na+ reabsorption and K+ secretion in the distal tubule
25. the loop of ________ has descending and ascending limbs
26. another term for urination
Down
1. the three functions of the kidney are filtration, reabsorption, and ________
3. the opposite of secretion
5. salt form of solutes most responsible for the hypertonic fluid in the medulla
8. Na+, Cl-, K+, and H+ are all known as ________
10. fluid forced out of the blood in the glomerulus is called ________
11. polymer of fructose used to measure the GFR
13. proximal tubule membrane surface with carriers for glucose and amino acid cotransport with sodium diffusion
14. positive feedback multiplication of solutes within the medulla to promote water reabsorption
15. ultrafiltrate buffer which is completely reabsorbed such that none is present in normal urine, normally
19. cytoplasmic extensions of podocytes found in the glomerular capsule
20. amino acids and ________are both reabsorbed in the proximal tubule by cotransport carriers
B. Essay
Essay Tutorial
This essay tutorial will answer the first essay question found in the “Review Activities” section of your Human Physiology textbook. Please read Essay Question 1. in the “Test Your Understanding of Concepts and Principles” section located at the end of chapter 17 and let me guide you through one possible answer. Watch for key terms in boldface type, helpful tips and general suggestions on writing the essay or short-answer questions. Enjoy!
94. Explain how glomerular ultrafiltrate is produced and why it has a low protein concentration.
Answer. Glomerular ultrafiltrate is produced by the hydrostatic pressure of the blood, forcing fluid out of the blood and into the glomerular capsule. This ultrafiltrate does not contain cells (too large) and very few proteins. Plasma proteins are often too large for filtration or are repelled by the negatively charged glycoproteins in the glomerular basement membranes. Two forces oppose the hydrostatic pressure of the blood: (1) the hydrostatic pressure of the capsule pushing back against the fluid being filtered; and (2) the higher osmotic (oncotic) pressure of proteins left behind in the filtered blood leaving the glomerulus. The higher oncotic pressure in the efferent blood attracts water away from the glomerular filtration capillaries. The blood pressure force is greater, however, such that the net filtration pressure at the glomerulus is approximately 10 mmHg, favoring the formation of filtrate.
I hope you understand glomerular filtration a little better after wrestling with this one. Now try a few more if time permits.
95. Explain how the glomerular filtration rate GFR is maintained fairly constant both by extrinsic (from outside) neural control and by intrinsic (local) autoregulation mechanisms.
96. Explain how 65% of filtered salt and water can be reabsorbed across the proximal convoluted tubule membranes without the influence of hormones.
97. Draw and label a complete nephron of the kidney. Describe three major functions of the kidney and highlight your drawing with examples of each function in action along the nephron.
98. Using your drawing from the previous question, describe the location of aldosterone receptors along the nephron and the effects of aldosterone on Na+, K+, and H+ concentrations in the body.
99. Explain the mechanisms that result in the formation of excess tissue fluid (edema) in patients with glomerulonephritis.
Answers — Chapter 17
- Structure and Function of the Kidneys
- 1. e, 2. b, 3. d, 4. e, 5. b, 6. b
- 7. F—Replace “intra-” with “extra-,”
8. T, 9. F‑‑Replace “pyramid” with “nephron,” 10. T, 11. F—Replace “medulla” with “cortex,” 12. T, 13. F—Filtrate forms urine in the renal pelvis
- Glomerular Filtration
- 14. e, 15. d, 16. b
- 17. T, 18. F—GFR = 180 L/day, 19. T, 20. T, 21. T
- Reabsorption of Salt and Water
- 22. b, 23. d, 24. c, 25. a, 26. b, 27. b,
28. e
- 29. T, 30. T, 31. T, 32. F—Replace “apical” with “lateral,” 33. T, 34. T,
35. F—Replace “hypo-” with “hyper-”, 36. T, 37. T, 38. T
- Label the Figure —Urea and Sodium Flow in the Countercurrent Multiplier System; See figure 17.18 in the text
- Renal Plasma Clearance
- 39. a, 40. e, 41. b, 42. e, 43. d, 44. e, 45.a, 46. c
- 47. T, 48. T, 49. T, 50. T, 51. T, 52. F—Replace “less’’ with “greater”, 53. T, 54. F—Only 20% of renal plasma flow is filtered, 55. T, 56. F—Switch 80% and 20%, 57. T, 58. F—Replace “hypoglycemia” with “hyperglycemia,” 59. F—D. insipidus is caused by inadequate ADH secretion from the hypothalamus
- Renal Control of Electrolyte and Acid-Base Balance
- 60. c, 61. a, 62. b, 63. c, 64. a, 65. e,
66. c, 67. e
- 68. T, 69. T, 70. F—Replace “proximal” with “distal,” 71. T, 72 T, 73 F—Replace “Na+” with “K+,” 74. T, 75. T, 76. T, 77. T, 78. F—Switch “bicarbonate” and “CO2,” 79. F—Replace “alkalosis” with “acidosis,”
80. T, 81 T, 82. F—Replace “carbon dioxide” with “H+,” 83. T
- Label the Figure — Plasma Sodium Homeostasis
- See figure 17.26 in the text
- Clinical Applications
- 84. e, 85. b, 86. d, 87. c
- 88. T, 89. F—Replace “proximal” with “distal and loop of Henle,” 90. F—Loop diuretics are among the most powerful diuretics, 91. T, 92. T, 93. F—Switch “Hemodialysis” with “continuous ambulatory peritoneal dialysis (CAPD)
- Chapter Review
Crossword Puzzle